Written by Maljini D Gunarathna
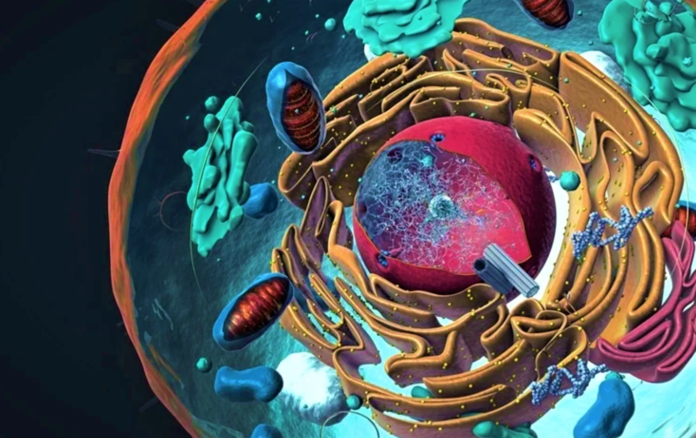
As we continue our journey into chromosome 6, we will take you through the diseases of the Human leukocyte antigen (HLA) system and how genetic research into this has led to ground-breaking testing and treatments. We have an exploration history with HLA genes as important targets in biomedical science and treatment. Within the 170 million base pairs, Chromosome 6 contains the genes that code for the Major Histocompatibility complex (MHC) system. MHC in humans is a region on chromosome 6 with hundreds of genes, including the HLA genes. This is an essential element of the immune system.
HLA genes code for the cell surface molecules on antigen presenting cells (APCs). These surface molecules are unique to each individual. Over the last 10 years, studies have correlated differential HLA expression levels with infectious and autoimmune diseases, cancer, neurological disorders, and drug hypersensitivity. Furthermore, HLA expression variation shows an impact on the outcome of transplants. Hence, we find that the clinical depth extends to various specialties like Rheumatology, Immunology, Hematology, Biogenetics, Pharmacogenetics, and much more through the process of HLA Typing. Understanding the intricacies of HLA typing opens doors to personalized medicine and targeted treatments, revolutionizing healthcare across diverse medical disciplines.
Applications of HLA Typing
As you will find out, HLA typing is an important section in understanding a wide range of genetically predisposed conditions and the factors contributing to transplantation and gene-targeted treatment.
HLA typing can be considered for:
- Recipients and their donors considered for hematopoietic stem cell (HSCT) or solid organ transplants
- Patients considered for treatment with specific drugs that have side effects associated with specific HLA alleles
- Platelet transfusion support for sensitised patients
- As a diagnostic tool for diseases associated with HLA
- Immunisation/vaccination trials
Within the last decade, rapid advances in Next Generation Sequencing (NGS) technology have resulted in innovative changes in medical genomics for applications in genetic diagnosis, called clinical sequencing. However, PCR-SSO and PCR-sequencing-based typing are still used as the first-line methods for HLA typing.
1. HLA typing for Organ transplantation
HLA typing is commonly used to decide transplant compatibility; since different individuals may have very different HLA alleles, which may cause alloreactivity (strong primary T-cell reactivity towards foreign MHC molecules). Solid organ transplant and HSCT both use HLA typing to determine compatibility. The greater the number of matched HLA loci between donor and recipient, the better the outcome of the transplant.
This is clinically significant, as the use of donors with allele-level mismatches affects survival and rates of ‘graft-versus-host disease’ (GVHD). Therefore, DNA-based allele-level HLA typing is used as the gold standard when unrelated donors are selected for transplant. During the rejection of an allogeneic transplant, the most immunogenic antigens detected were MHC class I and II molecules. The evidence indicates that the strongest determinant is HLA-DR, followed by HLA-B and HLA-A.
2. HLA typing for Drug sensitivity
HLA testing carried out for specific alleles linked with sensitivities to severe, sometimes life-threatening side effects of certain drugs, including abacavir, allopurinol, and carbamazepine is used to direct treatments with these drugs.
For example, hypersensitivity to abacavir is immunologically mediated. It is steered by MHC-I APCs through the activation of HLA-B*5701. Activation of HLA-B*5701 restricted CD8+ T-cells lead to the secretion of the inflammatory mediators TNF-alpha and IFN-gamma, generating the delayed-type hypersensitivity reaction (DTH). Abacavir hypersensitivity is regarded as a clinical diagnosis. Therefore, in North America and Europe, clinical guidelines recommend routine screening for HLA-B*5701 before going on abacavir treatment therapy.
The implementation of pharmacogenomics in routine clinical practice can improve different drug treatments. The advantages of the use of pharmacogenomics in clinical practice are,
- Assist in guiding the initial drug regimen
- Individualising the regimen
- Increasing efficacy
- Avoiding Adverse Drug Reactions (ADRs)
Moreover, pharmacogenetic testing is central when considering the economic resources of the patient or the public health system. Several studies have revealed cost-effectiveness when using pharmacogenetic biomarkers (i.e., HLA testing) to prevent ADRs in common drug treatments. In addition, there might be more HLA allele associations with ADRs in other ethnic groups that haven’t been studied yet. Therefore, pharmacogenomic research on this issue should be pursued. The HLA allele databases and the reports that assure the cost-effectiveness of HLA screening could assist future research on the pharmacogenomics of ADRs related to HLA alleles.
Currently, in the arsenal of approved small-molecule drugs, effective genetically targeted therapies for the treatment of autoimmune diseases are limited.
3. HLA typing to develop therapeutic strategies
Studies have revealed that an HLA variant’s preference for antigen binding and presentation causes the rise of T cells that recognise self-antigens, which have escaped self-tolerance mechanisms, to trigger autoimmunity. Research studies have demonstrated that if the presentation of an autoantigen to an HLA can be selectively disrupted, it can become a viable therapeutic strategy for autoimmune disorders.
Evidence shows several clinically significant autoimmune disorders linked to specific HLA alleles.
- Ankylosing spondylitis to HLA-B27
- Reactive arthritis to HLA-B27
- Psoriasis to HLA-C*06:02
- Rheumatoid arthritis to HLA-DR4
- Multiple sclerosis to HLA-DR2
- Type 1 diabetes mellitus to HLA-DQ2 & HLA-DQ8
- Narcolepsy to HLA-DR2 & HLA–DQB1*06:02
- Coeliac disease to HLA‑DQ2
Our evolving discovery platform continues to sharpen up the modelling of HLA-antigen and HLA-drug interactions, along with a growing collection of cellular and non-cellular assays. Nanotechnology in small molecule drug delivery and blocking genetic targets that are known to have a risk of disease development are key factors for future development in treatment therapies. They are vital in triggering the ‘autoimmune response personalized therapy’ approach for autoimmune patients carrying specific disease-associated HLA variants.
Future of HLA typing
The future of HLA typing promises to be an exciting and transformative journey in the realm of personalised medicine, transplantation, and immunology. As technology advances and our understanding of the Human Leukocyte Antigen (HLA) system deepens, several key trends and developments are shaping the landscape of HLA typing.
- Precision Medicine and Tailored Therapies: HLA typing is poised to play a central role in the era of precision medicine. With the ability to identify specific HLA alleles associated with various diseases, clinicians can tailor treatment strategies to individual patients. This personalised approach holds tremendous potential for improving treatment outcomes and minimising adverse reactions.
- Advancements in Technology: Next-generation sequencing (NGS) and high-throughput genotyping techniques are revolutionising HLA typing. These technologies offer higher accuracy, faster results, and the ability to sequence multiple HLA loci simultaneously. As these methods become more accessible and affordable, their widespread adoption is inevitable, further enhancing our ability to match donors and recipients for transplantation.
- HLA Databases and Big Data: The creation and expansion of comprehensive HLA allele databases will be pivotal. These resources will provide a wealth of data for researchers, clinicians, and bioinformaticians to better understand the complexities of HLA genetics and its implications for health and disease. Big data analytics will help uncover novel associations and patterns within the HLA system.
- Global Collaboration and Standardization: To ensure the widespread applicability and accuracy of HLA typing, global collaboration and standardization efforts will intensify. Harmonizing methodologies, data interpretation, and reporting standards will be essential to facilitate cross-border organ transplantation and drug safety assessments.
In conclusion,
the future of HLA typing is marked by an exciting confluence of technological advancements, personalised medicine, and improved healthcare outcomes. This field will continue to evolve, pushing the boundaries of what’s possible in transplantation, drug safety, and the development of novel therapies. As our understanding of the HLA system deepens, it promises to unlock new avenues for precision medicine and transform the way we approach healthcare.
Without a doubt, research into HLA and chromosome 6 is a significant topic that connects the fundamentals of immunology with clinical diseases. Through the development of research methods and technologies, we will expand our discoveries and broaden our prospects. On the horizon, we can see a future where HLA-typing methods will assist in realizing the goal of ‘precision medicine’ by identifying biologically distinct subgroups for precisely targeted treatments, giving hope to many who suffer due to the autoimmune responses of the human body.
References
Mungall A.J, Palmer S.A, Sims S.K, et al. The DNA sequence and analysis of human chromosome 6. Nature. 2003;425(6960):805-811. https://doi.org/10.1038/nature02055.
Delves P. J. Human Leukocyte Antigen (HLA) System. The MSD Manuals. Modified Sep 2022. Accessed June 21, 2023. https://www.msdmanuals.com/professional/immunology-allergic-disorders/biology-of-the-immune-system/human-leukocyte-antigen-hla-system.
Viatte S. Human leukocyte antigens (HLA): A roadmap. UpToDate. Last updated Mar 07, 2022. Accessed June 22, 2023. https://www.uptodate.com/contents/human-leukocyte-antigens-hla-a-roadmap#H6.
Nguyen H. D. HLA-B27 syndromes. Medscape.com. Updated: Apr 09, 2021. Accessed June 24, 2023. https://emedicine.medscape.com/article/1201027-overview.
Lázár-Molnár E. HLA testing. Arupconsult.com. Last Updated March 2023. Accessed June 26 2023. https://arupconsult.com/content/hla-testing.
Pediatric allogeneic HSCT (PDQ®). National Cancer Institute. Published February 4, 2022. Accessed June 26, 2023. https://www.cancer.gov/types/childhood-cancers/hp-stem-cell-transplant/allogeneic.
Nagy Z.A. Alloreactivity: An Old Puzzle Revisited. Scandinavian Journal of Immunology. 2012;75(5):463-470. https://doi.org/10.1111/j.1365-3083.2012.02680.x
Fricke-Galindo I, LLerena A, López-López M. An update on HLA alleles associated with adverse drug reactions. Drug Metabolism and Personalized Therapy. 2017;32(2). https://doi.org/10.1515/dmpt-2016-0025.
Torkamani, A. Abacavir and HLA-B*5701. Medscape. Updated Dec 07, 2018. Accessed June 25, 2023. https://emedicine.medscape.com/article/1969668-overview.
Sousa-Pinto B, Correia C, Gomes L, et al. HLA and Delayed Drug-Induced Hypersensitivity. International Archives of Allergy and Immunology. 2016;170(3):163-179. https://doi.org/10.1159/000448217.
Jeiziner C, Wernli U, Suter K, Hersberger K.E, Meyer zu Schwabedissen H.E. HLA‐associated adverse drug reactions‐scoping review. Clinical and Translational Science. 2021;14(5):1648-1658. https://doi.org/10.1111/cts.13062
Johansson T, Partanen J, Saavalainen P. HLA allele-specific expression: Methods, disease associations, and relevance in hematopoietic stem cell transplantation. Front Immunol. 2022;13:1007425. https://doi.org/10.3389/fimmu.2022.1007425.
Hosomichi K, Shiina T, Tajima A, Inoue I. The impact of next-generation sequencing technologies on HLA research. Journal of Human Genetics. 2015;60(11):665-673. https://doi.org/10.1038/jhg.2015.102.
Perni R.B, Schutte R.J. A new platform for HLA-associated autoimmune diseases. European Pharmaceutical Review. Published April 23, 2021. Accessed June 24, 2023. https://www.europeanpharmaceuticalreview.com/article/151719/a-new-small-molecule-drug-discovery-and-development-platform-for-hla-associated-autoimmune-diseasesLiu B, Shao Y, Fu R. Current research status of HLA in immune‐related diseases. Immunity, Inflammation and Disease. 2021;9(2):340-350. https://doi.org/10.1002/iid3.416.