Today, antibiotics have become the go-to pill irrespective of the ailment. This has caused the antibiotics to lose their effectiveness. After almost a century of being exposed to these killer antibiotics, bacteria have decided to grow through what they go through and evolve to resist the pharmacology of antibiotics. This phenomenon which is known as ‘antibiotic resistance’, has given rise to novel, untreatable infections caused by new strains of bacteria, classified as superbugs (Abushaheen et al., 2020).
Ways we contribute towards the development of antibiotic resistance
- Overuse of antibiotics by humans and animals
- Common antibiotics are bought without a prescription and used as first aid for infections that may not have a bacterial origin (Reygaert, 2018).
- The use of animal antibiotics in food-producing animals causes the risk of cross resistance with human antibiotics (McKellar, 1998).
- Improper prescription of antibiotic therapy (Reygaert, 2018)
- The choice of drugs may depend on low cost or low toxicity, rather than being appropriate for the infection.
- Prescribing broad-spectrum drugs as initial treatment.
Antibiotic resistance can be of intrinsic or extrinsic nature. Intrinsic antibiotic resistance occurs naturally. Some antibiotics are gifted with ‘antibiotic resistant genes’ that help to withstand the effects of antibiotics (Reygaert, 2018). Extrinsic resistance is acquired from bacteria with antibiotic resistance via gene transfer (Sagar, Kaistha, Das, & Kumar, 2019).
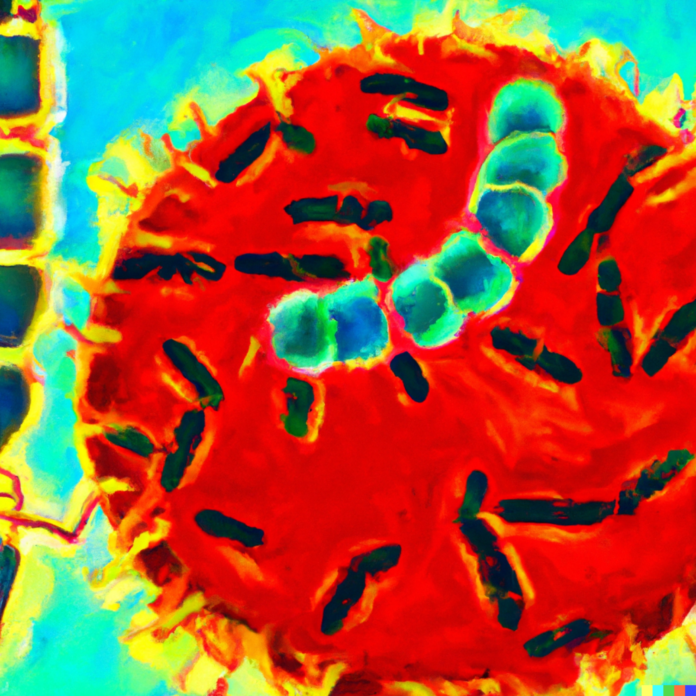
Figure 1: Schematic diagram of mechanisms of antibiotic resistance (Reygaert, 2018)
Mechanisms of resistance
- Limiting drug uptake
This intrinsic resistance mechanism allows the bacteria to naturally evade certain groups of antibiotics. For example, Mycoplasma spp. are absent from a cell wall. This gives them natural resistance against antibiotics such as penicillin and ampicillin, belonging to classes that target the cell wall of bacteria (Pandey & Cascella, 2022; Reygaert, 2018). Another interesting mode of limiting drug uptake is via the formation of biofilms. Biofilms are multicellular bacterial colonies of a single bacterial species or a variety of bacterial species. They are held together by a self-produced extracellular matrix which is thick and secure so that antibiotics cannot be reached (Lopez, Vlamakis, & Kolter, 2010). Furthermore, due to the bacterial cells being very close to each other, horizontal transfer of antibiotic resistant genes is frequent within the community (Reygaert, 2018).
- Drug inactivation
Drug inactivation is both intrinsic and extrinsic in nature. It can occur through drug degradation or by the transfer of a chemical group. For example, gram negative bacteria produce the enzyme, β-lactamases. The enzyme has the ability to degrade the most commonly used class of drugs that target the cell wall (commonly known as β-lactam drugs) via hydrolysis (Tooke et al., 2019).
- Drug efflux
Drug efflux is also common to both intrinsic and extrinsic resistance. Intrinsic resistance via drug efflux refers to the naturally present efflux pumps encoded by genes present in some bacteria to rid the cell of toxic substances or to transport compounds. Extrinsic resistance refers to induced expression or overexpression of the encoding genes, under harsh environmental conditions (Reygaert, 2018).
- Drug target modification
The final mechanism of resistance is strictly an extrinsic resistance mechanism. Due to the misuse of antibiotics, bacteria have been able to develop mechanisms to resist every class of antibiotics that were mentioned in part 1 of this series. For example, Staphylococcus aureus has undergone a mutation in order to change its cell membrane charge to inhibit the class of antibiotics that target the cell membrane. This enables the bacterium to resist the effects of the antibiotic (Miller, Bayer, & Arias, 2016).
Due to the short life span of bacteria, they are able to adapt and evolve under harsh circumstances. With the alarming rates of antibiotic misuse, it comes as no surprise that novel untreatable and severe infections are on its way. Rate of antibiotic resistance has grown so immensely that there is a high possibility that many newer mechanisms of antibiotic resistance have emerged in bacteria. Scientists are working on discovering new classes of antibiotics that can keep up with the rapid antibiotic resistance increase. Nevertheless, each of us individually is able to do our part in reducing its occurrence. Learn more about what we could do as individuals to reduce the rate of antibiotic resistance in the final part of this series.
Author: Esther Swamidason
References
Blair, J. M. A., Webber, M. A., Baylay, A. J., Ogbolu, D. O., & Piddock, L. J. V. (2014). Molecular mechanisms of antibiotic resistance. Nature Reviews Microbiology, 13(1), 42–51. https://doi.org/10.1038/nrmicro3380
Lopez, D., Vlamakis, H., & Kolter, R. (2010). Biofilms. Cold Spring Harbor Perspectives in Biology, 2(7), a000398–a000398. https://doi.org/10.1101/cshperspect.a000398
Qin, S., Wang, Y., Zhang, Q., Chen, X., Shen, Z., Deng, F., … Shen, J. (2012). Identification of a Novel Genomic Island Conferring Resistance to Multiple Aminoglycoside Antibiotics in Campylobacter coli. Antimicrobial Agents and Chemotherapy, 56(10), 5332–5339. https://doi.org/10.1128/aac.00809-12
Tooke, C. L., Hinchliffe, P., Bragginton, E. C., Colenso, C. K., Hirvonen, V. H. A., Takebayashi, Y., & Spencer, J. (2019). β-Lactamases and β-Lactamase Inhibitors in the 21st Century. Journal of Molecular Biology, 431(18), 3472–3500. https://doi.org/10.1016/j.jmb.2019.04.002
Abushaheen, M. A., Muzaheed, Fatani, A. J., Alosaimi, M., Mansy, W., George, M., … Jhugroo, P. (2020). Antimicrobial resistance, mechanisms and its clinical significance. Disease-a-Month, 66(6), 100971. https://doi.org/10.1016/j.disamonth.2020.100971
McKellar, Q. A. (1998). Antimicrobial resistance: a veterinary perspective. BMJ, 317(7159), 610–611. https://doi.org/10.1136/bmj.317.7159.610
Miller, W. R., Bayer, A. S., & Arias, C. A. (2016). Mechanism of Action and Resistance to Daptomycin inStaphylococcus aureusand Enterococci. Cold Spring Harbor Perspectives in Medicine, 6(11), a026997. https://doi.org/10.1101/cshperspect.a026997
Pandey, N., & Cascella, M. (2022, February 5). Beta Lactam Antibiotics. Retrieved March 2, 2022, from Nih.gov website: https://www.ncbi.nlm.nih.gov/books/NBK545311/
Reygaert, W. C. (2018). An overview of the antimicrobial resistance mechanisms of bacteria. AIMS Microbiology, 4(3), 482–501. https://doi.org/10.3934/microbiol.2018.3.482
Rouquette-Loughlin, C., Dunham, S. A., Kuhn, M., Balthazar, J. T., & Shafer, W. M. (2003). The NorM Efflux Pump of Neisseria gonorrhoeae and Neisseria meningitidis Recognizes Antimicrobial Cationic Compounds. Journal of Bacteriology, 185(3), 1101–1106. https://doi.org/10.1128/jb.185.3.1101-1106.2003
Sagar, S., Kaistha, S., Das, A. J., & Kumar, R. (2019). Extrinsic Antibiotic-Resistant Mechanism in Bacteria. Antibiotic Resistant Bacteria: A Challenge to Modern Medicine, 87–103. https://doi.org/10.1007/978-981-13-9879-7_7